Understanding Prostate Surgery: Prostatectomy, TURP, HoLEP, and Beyond
Understanding Prostate Surgery: Prostatectomy, TURP, HoLEP, and Beyond

Prostate surgery is a very effective treatment for many conditions. Here we take a look at prostatectomy, TURP, HoLEP and more.
Prostate surgery is a very effective treatment for several conditions, the two most common being prostate cancer and benign prostatic hypertrophy (BPH – also known as enlarged prostate).
In the case of cancer, these procedures are performed to stop the spread of malignant cells. For BPH, surgery may be required to relieve symptoms that are making it difficult to urinate, which can significantly impact the quality of life.
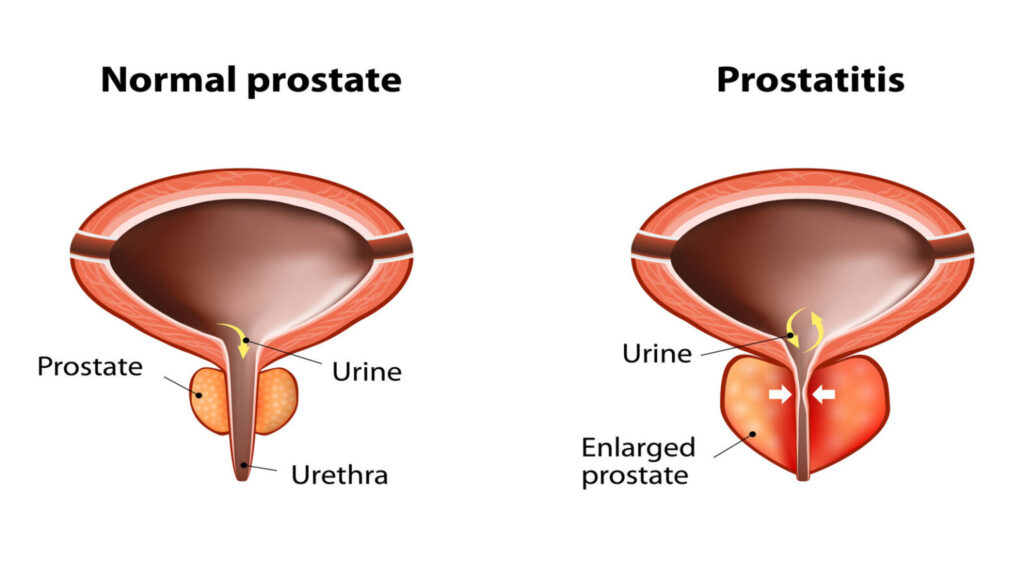
normal prostate and acute prostatitis.
What Is The Prostate?
The prostate gland is a part of the male reproductive system. Its main role is to produce semen, the fluid that carries and protects sperm. It is about the size of a walnut and sits just below the bladder in men.
The prostate is surrounded by the upper part of the urethra, the thin tube that carries urine from the bladder to the penis. It also carries semen from the prostate and sperm from the testicles to the penis during ejaculation.

The Different Types of Prostate Surgery
Prostatectomy
The term ‘prostatectomy’ describes several different surgical procedures to remove either part or all of the prostate gland. This may be required to treat prostate cancer or BPH.
When only a part of the prostate is removed, this is called a simple prostatectomy. This process involves enucleating it from its capsule to trim away excess tissue, but the sphincter muscle and nerves remain intact. It is usually used to treat BPH, a benign condition, meaning there is no risk of malignant cells having moved on to surrounding tissue.
When the entire prostate gland, capsule (or covering), the surrounding lymph nodes and neighbouring tissue is removed, this is known as a radical prostatectomy. This is usually a treatment for men with localised prostate cancer, and their many techniques used:
Open Surgery – This is where the prostate is removed via a large single incision in the lower abdomen or the perineum (the spot between the anus and the testicles).
Laparoscopic Radical Prostatectomy – The prostate is removed via several small incisions in the lower abdomen using small surgical instruments. This process is much less invasive than open surgery.
Robotic-assisted radical prostatectomy – Much like laparoscopic radical prostatectomy, the prostate is removed via small incisions in the lower abdomen. Robotic-assisted instruments are inserted through the incisions and controlled by a surgeon.
This allows for exact movements, meaning it is an even less invasive procedure overall. This has multiple benefits over open surgery, including lower blood loss, reduced hospital stay, and improved urinary control and erectile function after the operation. Dr Arianayagam is an expert in robotic radical prostatectomy and is one of the most experienced robotic surgeons in NSW.
Holmium Laser Enucleation of the Prostate (HoLEP)
Holmium laser enucleation of the prostate – abbreviated as HoLEP or laser prostate surgery – is another minimally invasive surgery. It is used to treat symptoms of BPH by removing blockages to urine flow.
This is achieved by inserting an instrument called a resectoscope into the urethra to get a visual of the prostate tissue and the lining of the bladder. Then a laser is used to cut away the obstructing tissue. Next, an instrument called a morcellator is used to cut the resected prostate tissue into smaller pieces. The tissue is then removed via the rectoscope.
Laser surgery is an effective way to operate on symptoms quickly and efficiently, and the procedure greatly reduces recovery time and postoperative complications.
Transurethral Resection of the Prostate
A transurethral resection of the prostate – abbreviated as TURP – is another operation to treat BPH symptoms by removing blockages to urine flow.
Rather than using a laser, the procedure employs a resectoscope into the urethra to get a visual of the prostate tissue and the lining of the bladder. Using the resectoscope, the urologist can trim away enlarged lobes of the prostate. The capsule of the prostate is left intact. This uses electricity as an energy source rather than laser energy.
Common Side Effects of Prostate Surgery
There are three main complications associated with prostate surgery: urinary problems, erectile dysfunction and sexual dysfunction.
With radical surgery for cancer, there is usually a period of incontinence that resolves within a few months. Therefore, pelvic floor exercises with a physio are essential before surgery. However, it can take several months for the incontinence to resolve, even with robotic surgery.
In severe cases, further surgery may be needed to treat incontinence. Erectile dysfunction is also a common side effect of cancer surgery and may take up to 12 months to improve. In some patients, normal function may never return. It is dependent on the preop function and the degree of nerve-sparing that can be performed (this depends on the type of cancer).
The side effect profile is much less after surgery for BPH (simple prostatectomy, laser or TURP). Some patients have some urgency or discomfort. The ejaculate is also usually reduced significantly. Erections are usually not altered.
Treating Prostate Surgery with Urology Specialist
Dr Arianayagam is a highly experienced urologist in Sydney and is an expert in all aspects of prostate surgery, particularly robotic radical prostatectomy.
Dr Arianayagam performs robotic radical prostatectomy at both Macquarie University Hospital and Nepean Public Hospital. Dr Arianayagam has performed over 300 robotic cases. In addition, he is a proctor for Device Technologies, which supply the Da Vinci Robotic System in Australia. Being a proctor means Dr Arianayagam is qualified to teach other surgeons to use this technique.
If you have any questions regarding prostate surgery or would like to book an appointment, please feel free to contact Urology Specialist here.
While you’re here, learn some more about how we can help you:
The Most Common Reasons For Erectile Dysfunction

Why Does Testicular Pain Persist? Common Causes to Know
Testicular pain is relatively common; however, when it becomes severe and long-lasting, there may be some cause for concern. This…

Everything You Need to Know About Sperm Health
It is not uncommon for men to have troubles with their sperm production, or to develop a sperm disorder. But…