Here we take look at the various types of testicular cancer, the causes and risk factors for men of all ages, and how it is diagnosed and treated.
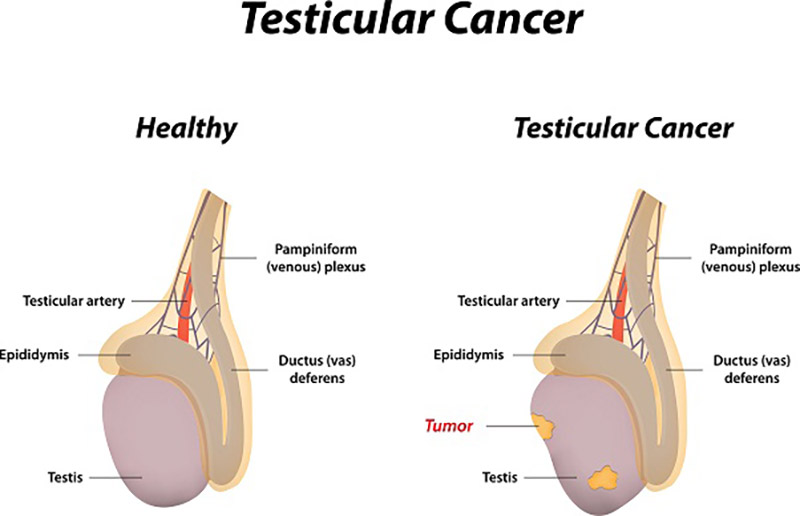
Testicular cancer is cancer that develops in a testicle, caused by abnormal growth of a cell in the testes. Usually only one testicle is affected, but it can affect both too.
The testicles are part of the male reproductive system. They have two main functions: to make male hormones such as testosterone, and to make sperm. The testicles are comprised of several cell types of which can develop into one or more types of cancer.
Types of Testicular Cancer
Germ Cell Tumors
Most cancers of the testicle develop in the cells that create sperm – these are called germ cells. There are two main types of germ cell tumors, seminomas and non-seminomas, each with their own sub-types.
Seminomas
Seminomas usually grow more slowly than non-seminoma cancers, and usually in men aged 25–45, but can occur in older men. There are two main subtypes of seminomas: classical seminomas and spermatocytic seminomas.
Classical seminomas are the more common variant and usually occur in men between 25 and 40. Spermatocytic seminomas are rarer and tend to occur in older men, they grow slowly and are less likely to spread to other parts of the body.
Non-Seminomas
Non-seminomas are rarer. That tend to develop more quickly than seminoma cancers and are more common in younger men between their late teens and early 30s. There are four main subtypes of non-seminoma tumours: teratomas, yolk sac tumours, choriocarcinomas and embryonal carcinomas.
There are three types of teratoma: mature teratomas, immature teratomas and teratomas with somatic type malignancy.
Most tumors are a mix of different types of tumours. Sometimes testicular cancer can include a mix of seminoma cells and non-seminoma cells.
Stromal Tumours
Some testicular tumours don’t develop in germ cells, but rather in the hormone-producing tissue of the testicles – the stroma. These are called stromal tumours. The two main types of stromal tumours are sertoli cell tumours and leydig cell tumours. They are usually benign and can be removed with surgery.
Intratubular germ cell neoplasia
Some germ cell cancers begin as a non-invasive form of the disease. The cells are abnormal, but they haven’t spread outside the walls of the seminiferous tubules, where sperm cells are formed. This is called carcinoma in situ (CIS) or intratubular germ cell neoplasia.
Secondary Testicular Cancer
Other types of cancer, such a lymphoma (cancer of the abdominal lymph nodes) can spread to the testicles. These are called secondary testicular cancers and are treated according to where they originated.
Causes/Risks Factors of Testicular Cancer
The exact cause of testicular cancer is not known, but there are certain risk factors that may increase a man’s risk of developing it. These include:
Undescended testes (cryptorchidism) – A condition where the testes do not descend into the testes after birth, but stay in the abdomen. This requires an operation to bring them down. Men with a history of undescended testes have a much higher chance of developing testicular cancer.
Previous case of testicular cancer – Men who have previously has testicular cancer in one testis have a 1 in 25 chance of developing cancer in the other.
Family history – Men with a male family member who has had testicular cancer have a slightly higher risk of developing it.
Infertility – Men with fertility problems (such as undescended testes) may have a higher chance of developing testicular cancer.
Symptoms of Testicular Cancer
Common symptoms of testicular cancer include:
• A lump on the testicles, which can be painful or painless.
• General pain or discomfort in a testicle or in the scrotum.
• Aching in the lower abdomen or groin.
• Backaches, coughing or breathlessness or tender nipples.
Diagnosis and Treatment of Testicular Cancer
Diagnosis
The tests used to diagnose testicular cancer include an ultrasound to confirm the presence of a tumour, bloods tests and removal of the testicle. Because of the nature of the cancer, a standard biopsy for the purpose of diagnosis is not possible as the procedure can further spread the cancer. If cancer is suspected then removal of the testicle is required. The removed testis is then sent off to assess the stage and type of cancer.
There are three different stages of testicular cancer. Stage one means the cancer hasn’t spread beyond the testicle. Stage two means the cancer has spread to the abdominal and pelvic lymph nodes. Stage three means the cancer has spread to other body parts.
Treatment
Treatment will depend on the stage of the cancer. For stage one cancer, removal of the testicle may be the only treatment required. This is known as an orchidectomy. Surgery, chemotherapy and radiotherapy may be required if the cancer has spread.
Treating Testicular Cancer With Urology Specialist
Dr Arianayagam is an expert in the field urological cancer surgery, including robotic surgery and laparoscopic surgery for the treatment of testicular cancer. He is widely considered one of the top urological oncologists in Australia.
If you have any further questions about testicular cancer and would like to book an appointment, please call Dr Arianayagam’s office on 1300 307 990 and his staff will be able to assist.