What Is a Prolapsed Bladder?
What Is a Prolapsed Bladder?
A prolapsed bladder can cause a number of issues with the bladder, and can be quite serious in some cases. Let’s take a look at some of the symptoms, causes and treatments.
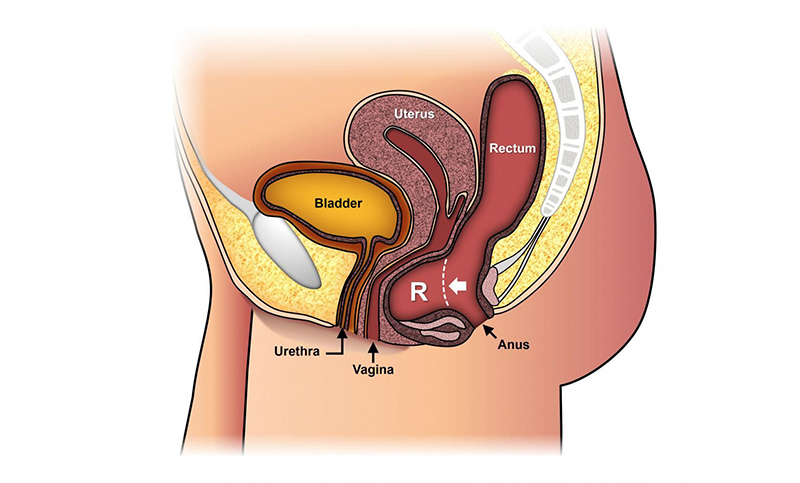
The bladder is a muscular sac located in the pelvis that receives and stores urine from the kidneys to be excreted via the urethra. For women, the bladder is held in place by the supportive structure of the pelvic floor and the front wall of the vagina. If this weakens, or if the tissue becomes stretched, it can cause the bladder to slip down and protrude into the vagina. This is known as a bladder prolapse.
It is quite a common condition, affecting roughly 30%-40% of women to some degree in their lifetime. And it is more more common in older women, or in those who have had child, or surgery to the pelvic region, such as a hysterectomy.
A prolapsed bladder (also known as cystocele) may cause a number of issues with urination. These will get worse depending on its severity (how far the bladder has descended into the vagina). There are four different grades for bladder prolapse:
• Grade 1 (Mild): Only a small portion of the bladder has descended into the bladder.
• Grade 2 (Moderate): The bladder has descended to within 1cm of the opening of the vagina.
• Grade 3 (Severe): The bladder has descended past the opening of the vagina.
• Grade 4 (Complete): The bladder has descended completely through the opening of the vagina. This is usually associated with another form of pelvic prolapse.
What Causes a Bladder Prolapse?
A prolapsed bladder is usually associated with some kind of strain to the pelvic region. Common causes include:
• Childbirth – This is the most common factor associated with bladder prolapse. The strain that childbirth places on the vaginal tissues and muscles can cause them to weaken, which affects the structures supporting the bladder. Having multiple children, or a particularly long or difficult birth can place you at a higher risk.
• Constant straining – Constant strain of the pelvic floor muscles, such as while on the toilet, from lifting heavy objects, strenuous exercise, or having a condition that causes you to cough constantly can all contribute to a weakening of the muscles.
• Other stressful factors – Such as obesity, pelvic surgery and ageing.
• Menopause – Levels of the hormone estrogen, which helps maintain the strength of the muscles in the vagina, begin to fall around menopause.
Symptoms of a Bladder Prolapse
Symptoms of a prolapsed bladder can range from very mild to quite severe, depending on the grade of the prolapse. The most obvious symptom is a noticeable bulge or lump inside the vagina that may feel like a ball is lodged inside it. This is often accompanied by pressure or a dragging sensation. Other symptoms include:
• Pain in the pelvis
• Difficulty emptying the bladder
• Bladder leaking during exertion (coughing, sneezing, exercise)
• The need to urinate more frequently
• Not being able to void the bladder completely
• Difficulty holding a tampon in place
• Painful sex
It is important to see your urologist if you have any of these symptoms. They may seem embarrassing, however they are nothing to be ashamed of and will likely only worsen over time. It is a very common condition and there are many effective treatments available to correct a prolapsed bladder – the earlier it is addressed, the better.
Diagnosing and Treating a Prolapsed Bladder
Diagnosis of a prolapsed bladder will usually involve a pelvic exam and questions about your medical history. Physical assessment will involve you lying down and straining or pushing to show the prolapse.
Other tests may include bladder or pelvic ultrasounds, urodynamics (a test to assess bladder function), a bladder scan after urination to assess how much urine is being voided, and cystoscopy (a procedure to get a visual of the bladder, usually to assess the best option for treatment).
Depending on the severity of the prolapse and the underlying cause, treatment will vary:
Conservative Management
Conservative management is suitable for mild to moderate cases. This may include:
• Lifestyle changes, such as weight loss or quitting smoking, if these factors are aggravating symptoms of the prolapse.
• Management of constipation, or modification of position while sitting on the toilet
• Pelvic floor muscle exercises (Kegels)
• Treatment of chronic coughing
• Estrogen replacement therapy
• Wearing a pessary – device that is worn to support the vaginal muscles. This needs to be changed every few months. It is more suitable for women who are not sexually active or who cannot have surgery.
Surgery
For more severe cases, surgery may be required to reposition the bladder and restore the support structures. Depending on the surgery, it will be performed under either a spinal anaesthetic, or a general anaesthetic. An incision is made in the vagina and the prolapsed area is strengthened with stitches. It may also be reinforced mesh or a skin graft.
Afterwards, a catheter will be interested to help drain the bladder. This will usually stay in place for 1-2 days while you are recovering in hospital. You maybe required to stay for up to five days. Full recovery usually takes up to 6 weeks. During this time you are not advised to do any heavy lifting or strenuous activity. In most cases, surgery is very effective at correcting prolapse.
If you have any questions about bladder issue or bladder surgery, please don’t hesitate to call and book an appointmemnt.

The Benefits of Drinking Water for Urological Health: Do You Really Need 8 Glasses a Day?
We’ve all heard the advice: “Drink eight glasses of water a day” But is this rule as important as it…

Protect Your Kidneys: Simple Habits for Better Health
Keeping your kidneys in shape is vital for reducing the risk of chronic disease. Check out some of our top…