Navigating Interstitial Cystitis: Understanding and Managing Painful Bladder Syndrome
Navigating Interstitial Cystitis: Understanding and Managing Painful Bladder Syndrome

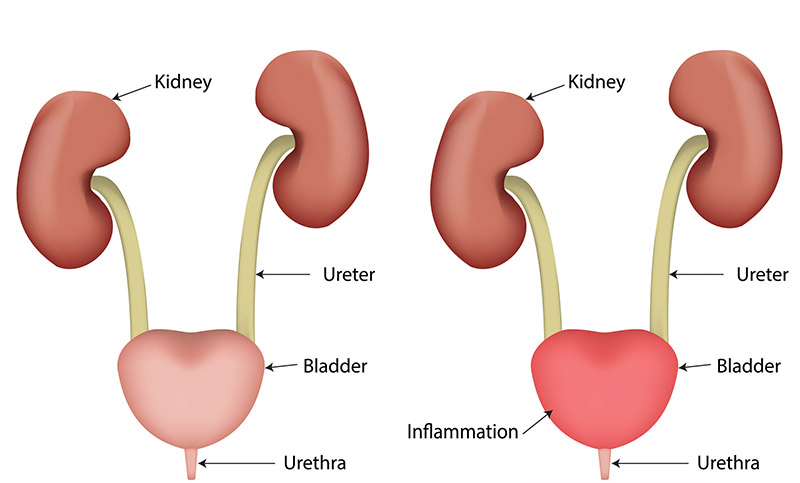
Interstitial cystitis – commonly referred to as painful bladder syndrome – is a urological chronic condition that causes pain and pressure in the bladder, and in some cases, severe pelvic pain.
IC can be a tricky condition as it is long-term, the cause is unknown, and diagnosis can be difficult due to it having similar symptoms to those of other bladder conditions. It is also far more common in women, with the ratio of incidence being roughly 1:10. Due to the severity in some cases, IC can have a real impact on the quality of life. However, there are treatments and medications that can offer relief.
What Is The Bladder?
The bladder is a muscular sac located in the pelvis, roughly the size of a pear when empty with a capacity somewhere between 400 and 600ml when full. It receives urine from the kidneys and stores it for excretion via the urethra.
It is a vital organ for keeping waste from building up within your body, and any disruption to this process due to poor bladder health can cause inflammation, bladder stones, infections, cancer, or incontinence, all of which can impact on your overall wellbeing.
Symptoms of Interstitial Cystitis
The symptoms of interstitial cystitis vary from case to case. For specific incidences, symptoms can range in severity and over time, hence why it can be difficult to diagnose. Symptoms can come on gradually, or abruptly for no apparent reason.
In mild cases, symptoms of IC can occur in “flares” in response to certain triggers. Because of this, it is often mistakenly self-diagnosed as a UTI. If you present any of the following symptoms, be sure to have a urine culture test.
• Pain or pressure when the bladder fills and relief when it is voided
• Urgent need to urinate
• Very frequent urge to urinate
• Only being able to expel a small amount of urine
• Pain in the pelvis or between the vagina and anus in women, and between the scrotum and anus in men; or chronic pelvic pain
• Pain during intercourse
How Is Interstitial Cystitis Diagnosed?
There is no single test that diagnoses IC, rather it is often a process of ruling other conditions or infections, such as urinary tract infections, an overactive bladder, bladder stones, bladder cancer, a sexually transmitted infection, endometriosis (in women), and BPH (in men).
The tests or procedures that may be performed to diagnose IC (i.e. rule out the above) include:
• Urinary culture samples to test for infection in the urine
• Cystoscopy – a procedure where a thin tube with a camera is inserted into the urethra to view the bladder
• Bladder hydrodistension – where the bladder is stretched with a sterile fluid using a cystoscope
• Biopsy – where a small piece of the bladder is cut out using a cystoscope for further analysis.
Treatment of IC
Depending on the symptoms, there is a range of treatment options available for interstitial cystitis. Generally these are implemented to help manage symptoms and return quality of life. Lifestyle factors and personal preferences will often influence what treatments are most suitable. These include:
• Dietary changes
• Quitting smoking
• Fluid intake management
• Physical therapies
• Surgery, such as a cystoscopy and hydrodistension
• Bladder training
• Medication
• Exercise
• Bladder instillations
• Nerve stimulation
Cystoscopy with Urology Specialist
While he is primarily a urological cancer surgeon, Dr Arianayagam also sees patients with general urological problems.
If you have any further questions about a condition or would like to book an appointment, please feel free to call 1300 307 990.

Understanding Kidney Stones: Causes, Symptoms, and Treatment Options
While most kidney stones will pass on their own accord, larger stones may require surgery. Here’s an overview of kidney…

Understanding Urinary Diversion: Three Types and Their Applications
There are three different types of urinary diversion, each applicable for different situations. Let’s take a closer look at all…